What services do you offer and how can we get in touch with you? Birth support is my main offering, but like many doulas, I have additional services as well. I offer postpartum care, abortion and loss support, placenta encapsulation, placenta prints using either blood or colorful India ink, and Bengkung belly binding for postpartum healing. I also have an online apothecary where I sell handmade herbal care products such as teas, sitz baths and salves. And you might see flowers pop up on my site from time to time! You can learn more about me and my business at Lunation Full Circle Care. Can you talk about what a Traditional Health Worker is and how it works to get OHP to cover doula care? Because doulas are such an amazing and effective way of improving better birth outcomes, a lot of states in the US are in various stages of providing reimbursement to doulas through Medicaid. There are currently 10 states with fully active programs and many other states are working on putting their policies into effect in the near future. Doulas in Oregon can become certified through the Oregon Health Authority as a Traditional Health Worker which then allows them to bill Medicaid for clients who have OHP insurance. In 2023, there was a sizable payout increase from $350 to $1500, which means that we are now able to serve more clients who might not have been able to access or afford doulas services otherwise. We are all very excited about the traction that doulas are getting these days and hope that it only keeps getting better! How can I find a doula who accepts OHP?
To find a THW doula, you can start by reaching out to your CCO (such as PacificSource, Trillium, CareOregon, etc.) to see if they have a list of doulas that are contracted to bill your particular OHP insurance. Community Doula Alliance is a wonderful organization that provides culturally specific doulas to the BIPOC community. Another great organization that has been serving Portland for many years is Gateway Doulas and they have a growing network of newer and seasoned doulas to choose from. I am a THW and am excited to accept OHP for doula clients at my business Lunation Full Circle Care!
0 Comments
Pregnancy, birth, and being a new parent are all intense experiences. They produce huge growing pains (literally and figuratively). They can carry immense joy, immense grief, complete wonder and total overwhelm, all at the same time. It's transformative and beautiful, but it's HARD. You can hold all of these emotions and sensations at the same time, but it's so much easier with community and mentorship. We weren't meant to do this alone and we don't have to. I'm Daniele Strawmyre, creator and owner of Ready Set Grow, a perinatal movement and education studio in Portland, Oregon. I’m a mother of three, a dancer and movement artist, a perinatal yoga and movement specialist, and the founder of Ready Set Grow. Originally from Philly, I'm an east coast transplant to the PNW trying to soften my sarcasm, a fierce advocate for neurodiversity and gender-affirming, unbiased, full spectrum, pregnancy and family support. I believe in the power of community. I genuinely love what I do. Everyone I work with does too. Ready Set Grow is an inclusive space for pregnant and postpartum people and their families. We use gender affirming and inclusive language and provide a trauma informed, nurturing, healing environment. We help people find strength and mobility during big physical, mental, and emotional life transitions.
To address my feelings of helplessness, and with a desire to be creative and connect with others in a time of isolation and collective trauma, I documented my pregnancy with weekly dance videos and related written blog posts, called Pregnant Pandemic Dances. Part journaling, part commentary on the scary and awful health and cultural events as they were happening…and a whole lot of humility and learning, I shared it on a website called Matrescence Monologues and on the RSG Instagram page. Throughout Covid lockdown (also my pregnancy and early postpartum period), I moved our classes online. Teachers from all over the country that I respected, and had learned from and alongside, offered prenatal and postpartum classes from their homes (their own children/babies/families sometimes interrupting). I taught and took many classes throughout my pregnancy and am so thankful for this lovely community, created out of necessity and adaptability. *We still offer a robust on-demand library from this time for anyone who can't make it to an in-person or live-streamed class. I birthed my third baby with the help of my amazing midwife Catherine from Unfurling Birth, my doula Megan of TenderEvolution, and the wonderfully kind and respectful team at Wildwood Birth supporting me and my family during the (hands down) hardest birth I've experienced. Even when things went off plan and we needed to transfer to the hospital, I felt respected and cared for. My last birth experience was a perfect example of how the right support can make all the difference. An unscheduled, emergency C-section during a pandemic is a recipe for trauma, yet my birth team held me so graciously, that I feel very good about my birth experience. In 2022, feeling the need for a physical community space for pregnant people and new parents, I reopened the RSG studio for in-person classes with fluctuating health & safety protocols in place. We've been building our class offerings ever since. When we started having wait-lists for classes, we added more to the schedule instead of increasing our class capacity to pre-covid numbers. We always want our classes to feel safe and community-building and that often means keeping classes smaller, leaving room for all that pregnant people, caregivers, and kids carry with them (physical, emotional, mental, and sippy cups). Some residual wisdom from pandemic times… I created RSG to fill a hole in support that I myself, felt as a pregnant person and new parent. Outside of the medicalized paradigm that is more generally available, there are vast and varied support options that are so often inaccessible or unknown to those navigating the transition to parenthood. Things like new parent support groups, movement for pregnancy relief, hands-on birth preparation, physical healing practices for the postpartum time, research based information, and a supportive community, are all important avenues of support that can be difficult to find, and are not usually “prescribed by a doctor”. As a new parent I struggled in all of the common ways. I also navigated serious health issues with my infant son while my mother was very ill. There were long stays in the hospital with my baby, traveling to Florida to care for my dying mother, years of therapy and health challenges for my son, and navigating the grief and then the inevitable loss as my mother succumbed to cancer. Although neither my partner nor I had any family nearby, all of these experiences were made more bearable due to a very active and supportive group of friends - our village. Community makes such a profound difference. In addition to all of these life challenges, I found myself unfamiliar with my postpartum body. As a professional dancer, movement teacher, and lifelong athlete, I was gobsmacked by the healing my body needed after birthing a baby. Even with all of my experience and knowledge, I struggled. Through a second pregnancy, grieving my mother, and a cross-country move to the PNW, I thought about what I wished existed as far as support and healing modalities for pregnant people, parents, their children, and their families. I looked for it in every state we stopped in, and couldn’t find it anywhere. So I created it.
Our teachers have extensive training in the physiology of birthing bodies in their varying stages. In addition to the education and knowledge they share through movement, our teachers are collectively doulas, nurses, midwives, occupational and massage therapists, lactation consultants, and bodyworkers. We're the only yoga and movement studio in Portland, Oregon that focuses solely on pregnant and postpartum people, parents, kids and families. We are committed to being a judgment-free, safe space for ALL families regardless of race, ethnicity, religion, ability, or gender identity. We embrace neurodiversity, gender fluidity, bodies of all sizes and abilities. We support all birth choices and outcomes. We focus on the specific needs of pregnant and postpartum bodies in all of our adult classes. You can view our schedule and sign up for classes at www.andreadysetgrow.com/class-schedule Cheers, Daniele Currently, we have movement classes every day for pregnancy and for postpartum, plus classes for parents of mobile babies and toddlers, (because why doesn't this exist already)?! Plus, baby-wearing dance classes, core and pelvic floor retraining and support, classes for young children, so many things. Offerings like:
This is a wild time in the world and we know many of you have questions and concerns about Covid-19 in relation to pregnancy, breast/chestfeeding, conception, etc. While there are some things we know, unfortunately, there is still much to learn about this virus. Check out this link for the most up-to-date information about Covid-19 and pregnancy and breastfeeding from the CDC here.
First things first, we want you to know that we will continue to be available for prenatal care, births, postpartum care, and fertility support throughout this tumultuous time. We know that many people are wondering if a home birth might be a safer or more comfortable option at this time and we are open to talking to you, answering your questions, and accepting late transfers to care for this reason. We are also available to offer prenatal care (in our office) and postpartum care (in your home) to clients who want to continue with their plan to have a hospital birth who may want to avoid going to the hospital or clinic for the time being to limit their exposure. We will continue taking many precautions to help prevent the spread of this virus, which include: 1) Encouraging our clients to take social distancing seriously, to stay at home when they can, and practicing this ourselves when we are not providing direct care to our clients. 2) Washing our hands before and after each visit and asking our clients to wash or sanitize their hands before coming in to the office. 3) Cleaning all high-touch surfaces and equipment in our office in-between visits. 4) Staggering appointment times so that clients don't have to come in close contact with each other and we have more time to clean in-between appointments. 5) Offering online, easy to use, HIPPA-compliant telemedicine appointments when appropriate. 6) Ensuring that our clients and their family members are all in good health before doing in-person appointments to limit our exposure to illness. 7) Temporarily removing the children's toys/books from our office and asking our clients to leave their children at home for appointments whenever possible. 8) Recommending hospital birth if anyone has symptoms of Covid-19 when they go in to labor. 9) Not having direct contact with clients ourselves if we are at all sick. If you are interested in the possibility of transferring care to a home-birth midwife, or want some out-of-hospital prenatal and/or postpartum care, feel free to call us anytime at (503) 310-9715 or fill out our contact form here. We would be happy to set up a free online video or in-person consultation. This is a chance for you to get all of your questions answered, hear what care with us would look like, and see if we'd be a good fit for you and your family. We are holding our pregnant, postpartum, and trying-to-conceive clients close to our hearts during this time and wishing good health for you and your families. We will do our best to continue to provide you with more information about this virus in relation to pregnancy and breast/chest feeding as it becomes available. Who is Birth First Doulas and how long have you been around? Birth First Doulas is a labor and birth doula agency here in Portland, Oregon. Our goal is to help wonderful families and wonderful doulas find each other! Over the last 25 years of attending births and training doulas, we’ve watched the demand for doula services grow and grow but have not seen an equal expansion in systems and businesses that support doulas to provide their services. Our Birth First vision is to be Portland’s most trusted doula agency and to provide the business framework, professional standards, and reliable reputation from which families and doulas both benefit. Brooke Noli and Rebecca Durlin Smith are the co-owners of Birth First Doulas, and although we have 25 years of combined doula work experience, our Birth First Doula agency has only been up and running since May, 2019. We are amazed at how quickly the agency has grown and delighted that doulas are increasingly in demand as more and more people learn about the benefits of doula care. What services do you offer? Birth First is primarily focused on providing birth doula services. We believe that specializing in one skill refines that skill, so instead of trying to offer every service related to pregnancy, birth, and postpartum, we decided to specialize in high quality birth doula services. Our comprehensive doula package includes all the following services to support families on the journey to their baby:
What are the different classes you offer and how can I find out more details?
We offer two childbirth education classes and one newborn sleep class. Each class is 2 hours long, offered once a month, and can be taken together or individually. Here are the details: Stages Of Labor Crash Course: The Birthing Process This class provides parents with an in-depth understanding of the birthing process, which includes the stages of labor, birth, and the immediate postpartum. Classes are dynamic and interactive to keep you and your birth partner engaged, laughing, and connected. When: The first Sunday of every month from 1-3pm Fee: $80 for two people. Free for Birth First Doula clients (must still register). Teachers: Kelly Turner & Bri Dewey Location: At the Brand New Birth First Doula Space: 7800 SW Barbur Blvd. #3, Portland, OR 97219 Register Here Labor & Birth Techniques: Balancing Progress, Comfort, & Relaxation This class provides parents with insider information and tips on everything you need to know about comfort techniques, labor progression techniques, and creating a calmer, more satisfied birth experience. Classes are dynamic and interactive to keep you and your birth partner engaged, laughing, and connected. When: The first Sunday of every month from 4-6pm Fee: $80 for two people. Free for Birth First Doula clients (must still register). Teachers: Kelly Turner & Bri Dewey Location: At the Brand New Birth First Doula Space: 7800 SW Barbur Blvd. #3, Portland, OR 97219 Register Here Newborn Sleep Class: Creating Gentle Sleep Rhythms During the “4th trimester” you are getting to know your baby. It’s too early to start sleep training but it’s never too soon to start creating a healthy routine to get you and your baby sleeping. This class is taught by sleep trainers from Full Circle Sleep and will teach you all about soothing, natural circadian rhythms, and developmental milestones to help you thrive in these first 4 months. By the end of the class you will know how to establish a foundation of healthy sleep hygiene, be familiar with safe sleep guidelines, and understand what you can do now to create excellent sleep habits that last a lifetime. Offered once a month and taught by certified sleep trainers who are also Birth First Doulas. When: Every month on a Sunday from 1-3pm Fee: $100 for two people; free for Birth First Doula clients (must still register). Teachers: Camilla Rae & Atika Hagen Location: Portland Pediatric Acupuncture, 1703 SW Clay Street, Portland, Oregon, 97201 To Register: Contact [email protected] And Stay Tuned for upcoming classes on Feeding Newborns and Newborn Care 101! How can a doula be helpful for a home birth? Lots of people think that doulas are not needed at home births, but our experience is that a doula is a valuable asset at any birth experience! While it’s true that home birth midwives offer excellent continuity of care and connection, their role is still quite different than a doula’s. During pregnancy, doulas can make space to talk about all the things that there may not be room for in your prenatal appointments with your midwives and we can really dig into the topic of labor support and what will be most helpful when the time comes. As doulas we do not have to provide any medical care so we can be 100% focused on the mental and emotional experience of you and your partner. While your midwifery team is doing the important work of monitoring your baby, charting your progress, and preparing for delivery, we can focus in on comfort techniques, labor progression, birth support, and helping your birth partner to be as present and connected as possible. Doulas often arrive before the midwives to offer early labor support, and once the midwives do arrive there may come a time when they need to get some rest in order to stay alert for your medical care. We can also assist with taking photos, preparing food, caring for pets, or other tasks that may be helpful to you when the time comes. Home birth clients also get to take advantage of all the Birth First Bonuses that we offer like complimentary childbirth education classes, newborn sleep classes, new parent support groups, and discounts on spa services like massage, acupuncture, chiropractic, and much more! How can I contact Birth First Doulas? The link to our website is: https://www.birthfirstdoulas.com The link to our contact page is: https://www.birthfirstdoulas.com/contact/ Our phone number is: 971-361-6833  Rosemary, how did you first get involved with birth work? My inspiration to become a birth worker came like lighting. In my early thirties my life took a 180 degree turn in my career path. Back in 2008, I had the opportunity to meet Rita Aparicio, a Puerto Rican traditional midwife and founder of Doula Caribe International. After completing Doula Caribe's doula certification facilitated by her and other local providers in the area, I knew birth work was my destiny. Soon after, in 2009, I founded Simple Touch of Life providing doula services, prenatal/postpartum massage, childbirth classes, and lactation support. What was your experience of birth in Puerto Rico like? Most of my birth work support from 2009 to 2013 was in hospitals in the San Juan metro area. More than 98% of births on the Island are performed in hospitals with a cesarean rate of 44%. Back in that time, the majority of the OBs attending births were trained with a very patriarchal and bigoted mindset. In 2009, the doula concept was still a foreign term for most hospitals in the area. This lack of knowledge made it hard and unpredictable for doulas to offer their services. There were times that I had to identify as a family member to prevent not been kicked out of the labor room and be able to advocate for my clients. Many times during labor, I witnessed my clients being harassed and bullied by their providers. Obstetric violence is not a myth - it's real! This caused so much trauma for the pregnant person and their families in a moment where love, safety, and respect should be the norm. There were very few OBs that understood the benefit of having a doula and how our presence and advocacy enhanced their client's birth experience. It was amazing on the rare occasion when everyone was on the same page and worked as a team towards the same goal - for our pregnant families to have a dignified and safe birth. With the hard work of local doulas, the government approved a law that protects Puerto Rican pregnant people to choose who they want to be with them during their labor, including doulas. These experiences inspired me to become a midwife. This shift in my birth work journey provided me the opportunity to work with local Puerto Rican midwives and witness the power of the Midwifery Model of Care. We are so excited to have a midwife of color on our team and we all know that birth outcomes for POC are much worse in general than for white people in the United States. How do you think midwifery care can serve POC and help turn this around? It is all about taking the extra step and educating ourselves when caring for our POC communities. It can not be defined in one sentence. We all have complex and rich cultures with many layers of history. Some basic suggestions: 1) Stop assuming. Assumptions can create a missed opportunity to have a better understanding of your client's health and build trust. For example, first generation native Spanish speaking clients (White, Black, Brown) can be from South or Central America, the Caribbean, or Europe. This means that we have a common language, but DIFFERENT diets, beliefs, cultures, history, health care, body structure, hair texture and so much more. 2) Learn more about the particularities for genetic conditions that are more common in particular ethnic groups. For example, a black person from Angola will be at a higher risk for having different genetic conditions than a black person from Cuba. This goes back to number one, do not assume! 3) Help access quality and equality of care in hospitals. BE AN ADVOCATE!! What do you love most about being a midwife? There are so many things that I love about being a midwife but at the top of the list is how the Midwifery Model of Care is about so much more than merely facilitating a birth. It is about reproductive and human rights! It is about providing the freedom and safety for pregnant people to have individualized care no matter their race, social status, sexual orientation, gender, or religion. Midwives rock my world!! Is there anything else you'd like to share? I want to send a shout out to all the midwives of color! Thank you for standing strong and making a difference. Sisters... I celebrate you!!
 "Labor was a long wait to come - 41 weeks and a day (Nov 25), to be exact. I felt some light surges come and go just an hour or two before Jay came home. I didn't pay any mind to timing until he had been home and I was on my way to my 5 o'clock chiropractic appointment. Between the time I walked out the door and the time I got to my appointment, about 15-20 minutes, I had had 3 surges. They were a bit stronger than earlier but I wasn't getting my hope's up, just rolling with it. While at the office, I had 1 before the adjustment, 1 during, and 1 before leaving. When I got home, I let Jay know. I got the kids to bed and let my doula and midwives know that I was going to take a bath and try to get some rest in case it was the real deal. It was about 8pm now. I relaxed so well in the bath I almost was falling asleep, so I decided to hop out. As soon as my belly hit the air, another surge rolled in and a strong one, strong enough I had to wait to get out. Once I was out as I was trying to dry off, another one hit. At this point I was bent over leaning into them. I gave up on my after-bath routine and threw on a nighty and created a nest in my bed, checking back in with the midwives/doula about the outcome. I struggled to get comfortable, the surges kept coming. As Jay and the kids slept, I got up and worked through the surges alone and in the dark. I labored in our room, in the bathroom, and in the living room. The surges grew stronger and more frequent. Finally, I had to wake Jay to message our doula. A few surges later, I had him call them both. The doula showed up in about 45 minutes, about 11:30/45pm and the midwives came in about 12:30/45am (Nov. 26). To get an idea of where I was at, since I have history of long labor and slow progression, I allowed a dilation check around 1:30am. I was 4cm. I labored around, on the floor, my yoga ball, the bathroom, the couch. My doula helped me do some counter pressure on my back and hips, some side lying releases and get comfortable on the couch to rest. Sleeping in between each surge, getting support through each rush, I napped about 30 minutes each side. Around 3:00am I was checked again and was happily AND nervously at 6cm. So many emotions and thoughts I had in my head, since I had never made it passed 6cm with the boys. But I was quick to hush them and fill my mind with positive, affirming thoughts. Eli (my son) woke up around this time. He visited with the birth team and gave his momma love. Now, resting reclined, I was quick to sit up and call for Jay's assistance with each rush. It was getting intense and I needed his strong arm to pull on and I moaned a low moan as I felt called to. We all talked and joked and laughed. Especially trying to get me to the bathroom to pee each time, as I could never make it in time. Half way there, every time (right in front of the kitchen), another rush would come and I would pee. On the floor. In the same spot. Every. Time. I couldn't believe it. Logan (my 1 year-old son) had slept through this all and finally woke about 7:30am. Around 8:00am, I got in the shower and sat on my yoga ball. Eli's favorite part, he got to hold the shower head and run the water over my back and belly. He was so proud. The water was like magic, I even claimed so in the moment, as soon as it hit my belly it was instant relief. Even through the waves, I was relaxed. And when I got out, I felt energized. The boys ate and played and became too full of energy, so we sent them to the neighbors' I think around 9:00 or 10:00am? By 11:00am, I was feeling SO good and we decided to check my progression again. I. COULD. NOT. BELIEVE. IT. I was 8cm!! My midwife asks me, "How does it feel to be 8cm? You ready to fill up the pool?" I said, "I would LOVE too, but I actually think I could run a mile first!" I could not believe how GREAT I felt and to be so close to the end stage of labor.
The surges were enough to wake me up and get me in a deep moan and occasionally call for Jay's support to get through, but were also very spaced apart. The longer I rested in the warm water the longer the spaces got between them. After an hour or so of rest, I was called out. The midwives were afraid to let my labor stall too much. Once out of the water, that's when labor REALLY hit me. I was growling at points and when it felt too much, I was calling out to my baby, "We ARE doing this, my baby." When the pressure was too intense, I breathed down, "I feel you coming" "Come down, my baby". When I felt weak, I growled, "I AM strong." "I CAN do this." At this point, every rush I was begging for Jay's support. And every time, he was there. 3:00pm rolls around, and since I was in active labor and a "high risk" home birth, I was checked again. Still 8cm. With the lack of progression after 4hrs, my midwives were uneasy. They came to me and suggested a transfer. They expressed concern of prolonged intense contractions on my 13mo (and stretched) uterine scar tissue and the possibility of this stage lasting several hours more. They felt strongly the need of a light epidural, to allow my body to rest. She reassured me that she would call all of the nearest hospitals and seek out the most supportive hospital with the most supportive staff, while giving Jay and I a moment to talk about it. I was in shock. Jay was on the side of the best option to be sure to have a safe and healthy momma AND baby. Me. I was scared. I didn't want to go. I felt this was me giving up. I felt my hard work was all put to an end. That I was loading up to sign my birth rights away for some strange doctor to surgically remove my baby. The ride there was treacherous. Wading through Portland traffic, in RUSH HOUR. Getting to the hospital, riding in a wheelchair, getting undressed and onto a hospital bed, laying there on my back, being hooked up to monitors, being asked a million questions over and over again. Moaning, begging, fighting my way through the rushes. I was out of my zone. Fear had set in deep, despite the AMAZING staff that cheered me on and constantly reminded me they were on my side and that I was GOING to do this, and the pain began to be unbearable. I could. Not. Wait. For an epidural at this point. We checked into the hospital around 5:00pm and the epidural was placed around 7:30pm.. By now my once excited son was now scared, and of me. He thought the doctors were hurting me. He didn't want me to have a baby anymore. He didn't want mommy to be in pain. He wanted to go home. I reassured him the best I could.. A little while later my birth team and I discussed my options with the midwife on staff. I was adamant to not have pitocin to augment my labor. Since my waters had not yet released, I agreed that would be our first line of action. And if that didn't take us anywhere we would seek other options before pitocin (such as pumping). At 9:00pm she ruptured my waters. During this time, my midwives and doula went and got snacks and tried to entertain the kids. Without even asking (because I knew the hospital's answer), I demanded snacks from my own crew. I released my doula sometime between 10:00 and 11:00pm, figuring having my midwives here would be enough. Jay worked to get Logan asleep and Eli was finally comfortable enough to lay beside me. I layed quietly in my dim room trying to commit to a nap, but it wasn't happening. My mind was racing. Thinking of all the possible outcomes. Finally, Jay got Logan to sleep and Eli was asleep beside me. MY midwife, Catherine, snuck in. She helped reposition me on my side and we quietly talked. About my feelings and where my head space was at. It was a good, intimate moment. She moved Eli and sat quietly beside me. Jay resting in the other chair. It wasn't long before the pressure down below became uncomfortable and I was feeling the need to sit directly up with my knees up as well. Catherine helped me get into position and called the midwife on staff, letting her know my sensations. After a check, I was 9cm with a slight cervical lip, in which she manually pushed back. An hour later, the pressure was REAL. I have never felt the need to poop so bad in my life, haha.
I had not prepared for an epidural birth, so I had only practiced birth breathing/breathing down, and had to be coached and awkwardly taught how to push. I was feeling like it was impossible and I was reminded - that means I was almost there. I kept telling myself, "this is good." As the feeling of my body separating (opening) felt impossible. Logan woke up, just a few contractions before Kayden's head emerged and what a relief that was! A few more contractions and I hear the midwife say, "I am going to pull him out, okay." Instantly, I say, "No! Don't pull him out." And the reply is, "It's okay, I am just going to pull him out." As she pulls and twists Kayden from my body and lays him on top of me (12:06am Nov 27). He is out. Having an out of body experience, I am looking down.
Interview with stephanie elliott of elliott lactation and education - education classes for parents!4/17/2019 Stephanie, can you tell us a little bit about yourself, personally and professionally?
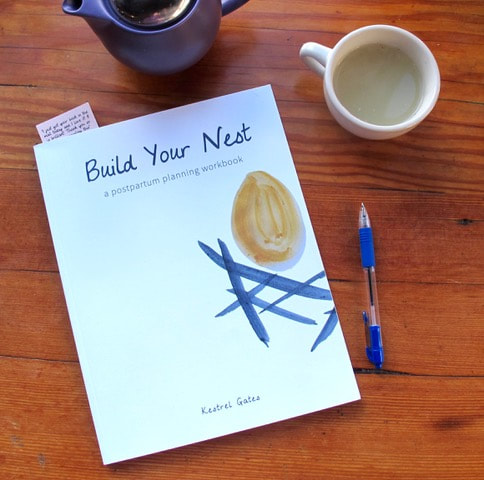
I’m a 32 year old midwife, lactation consultant, educator, mom, and eternal student. I was raised in rural Ontario, Canada, then moved to Montreal in my late teens and attended my first birth at 19! I worked as a doula primarily with immigrant and refugee populations. I learned a lot about humility and women’s courage during that time. At age 22 I moved to Portland to become a midwife. I went to Birthingway and did my clinical training at Alma Birth Center where I then went on to become an assistant and eventually a lead midwife. In my time at Alma I developed my love of clinical care —problem solving, collaborative care, researching evidence-based practice, and obviously catching babies— but I also developed my love of education and informed choice. Midwifery is always a process of shared decision-making: the midwife giving their best information about safety and personally deciding what they are comfortable with, and the client deciding which procedures, tests and screens they want to do, and ultimately what risks they are willing to take for their own family. In order to make those decisions from a really grounded place, people need excellent education, so I found that I loved helping my clients truly deeply understand things so they could make decisions guided by their own values and risk-assessment. I also LOVED teaching midwifery students. After 7 years of being on call and catching babies I decided to return to school. I loved being a midwife, but I had concerns about my ability to be on call 24/7 and care for the family I hoped to have soon. Additionally, I was becoming more and more aware of the startling statistics about inequities in maternal child health in the US and wondered if I could be more involved in finding a solution to that. I begin my masters program in Epidemiology in the fall and I’ll specifically be looking at disparities in birth outcomes for babies and moms. It’s really important that we gather lots of data about how racial discrimination and oppression specifically impact birth outcomes to create targeted interventions to stop it and make birth equitably safe for everybody. While I was in school I started to teach childbirth education, newborn care, and breastfeeding classes at Legacy. I just left that job to focus on my education business, because I just wanted to be able to focus on things I think are neglected in most childbirth education classes. How has becoming a parent changed your relationship with your work? Well, I’ve never been a very dogmatic midwife. I’ve never had strong opinions about how people *should* give birth because birth is so personal and we all have our own stories and traumas and preferences, so I’ve never been a huge advocate for natural birth, or a certain method of birthing or parenting. I’m like, ‘natural birth is great! Let’s do it! But also epidurals are good too! Have one if you want! Breastfeeding has lots of benefits and is great food for babies, but if it’s going to give you dysphoria or make you want to crawl out of your own skin to do it, don't! Let’s learn about bottle-feeding!’ I guess having a baby made me feel even more like that. It made me more pro-choice, and even more like ‘hey, you should do this in the most you way possible’ because you are the right parent for your kid. When I was gearing up to have my baby a lot of well-meaning midwife friends who’d given birth were like “you just have to get out of your midwife brain and be in your body”. This seemed like pretty good advice, right? Like, based on what we know about the hormones of labor it’s good to be relaxed and in your “lizard brain” not thinking much. But, listen... I’m incredibly cerebral. My brain is my best companion and there was no getting out of my head. So I used my brain during labor. I created my own mental activities to get myself through the intensity of labor because that was the most me way to give birth. So, I guess I want to help people tap into their own most me way to give birth. Like, my way probably won’t work for you, you know? My grounding philosophy about birth is that I want everyone to feel educated, empowered, and supported, and like they understand what is going on. Beyond that, people can use their own values, beliefs, and personalities to guide them through birth. They don’t need me to impose mine. I haven’t caught any babies since I gave birth and I probably won’t again unless I get really lucky on an airplane or the apocalypse happens, but if I did I’d probably hold those birthing folks a little closer, see them through a few more tears in my eyes, and be filled with the absolute deepest thrill for the adventure that was yet to come. Tell us a little bit about your classes! I'm so excited about these classes! I’ve been teaching childbirth and parenting ed for threeish years in the hospital and it’s been great fun. I was actually really impressed by the quality of the classes compared to my previous assumptions about what hospital classes were like. Props to Legacy. They’re doing a good job. But I really wanted to make my own curriculum that allows for inclusion of some things that I think aren’t always prioritized. I’m really into helping people understand the mechanics and physiology of birth, partially because I’m a giant nerd, but also because I think it really helps so I offer some great hands on models and materials to help people understand what’s really happening. I think I offer a little more science with my birth classes just because I’m endlessly in awe of it. But I also wanted to emphasize recovery more. We live in a country with ZERO WEEKS of paid maternity leave, our expectations of human bodies and human hearts are completely unreasonable, so I do my best to give people the best information about how to recover physically and emotionally from birth and begin to function in a society that is more or less outright hostile to new motherhood. I focus on postpartum planning a lot, because I think we don’t emphasize that enough. I was excited to see that you interviewed Kestrel Gates because I LOVE her workbook and the deliberate attention to postpartum planning. Generally my classes are dynamic, fun, and simultaneously reverent and irreverent. I make bad jokes. I focus on a lot of kinesthetic learning tools, so we practice positions for labor and skills like swaddling and baby-wearing, and I also have physical models of things that we can pass around and touch and you can open a cross section of a uterus with your own hands and begin to understand what it means to have this organ in your body. Again, I’m not pushing any kind of dogma, so my classes are appropriate for folks birthing in all settings with all plans for pain management, without any judgement from me. Likewise, people of all gender identities, body sizes, races, cultures, family structures, abilities, etc are going to feel comfortable in my classes. The class I’m most excited about is one that isn’t really offered elsewhere and its based on a major need I see not being met right now. That is my “Understanding research and informed decision-making for parents” class. That’s a mouthful but what it is, essentially, is science literacy for the internet age, specifically as it pertains to parenting (although the skills learned in this class can apply to research in all facets of life). It’s a class that helps you in the situation where you’re with a friend and they say “well I read that *** is really dangerous and that we should do this *** instead” so then you can then say “ok that’s really interesting, I should research that” and then have the skills to know which of the information you find on the internet is based in science, whether the science is good, and how to weigh the information and make your decisions. Likewise, what do you do when NPR reports on a study that says that everything we thought was true about something isn’t. What do we do? Do we change course? In this class I’m not proselytizing against natural medicine, or for vaccines or anything like that, I’m just trying to help you access and assess information and make decisions based on a combination of good information and an understanding of its sources, your personal values and ethics, and what feels right for your family. I’ve had a huge amount of privilege to be able to learn these skills in my degree and I’d just love to share them with parents. Also the class will be SO FUN and not stuffy. One last thing: I use an online learning platform to supplement the in-class education. So in addition to our class time students can log in and see tons of resources, videos, and have an opportunity to build community and engage with their classmates if they so choose. What can parents hope to go away with from your classes? Confidence, mostly. I want them to feel confident in their knowledge and skill-set, in their ability to cope with the intensity of labor and the curve balls labor and parenting throws their way, in their decision-making skills, and confidence in themselves, their families, and their relationships to grow stronger through this intense transition, rather than to suffer. Also, excitement, because parenting is incredible. Also deep self-acceptance, because I’m all about people just being their damn selves and being ok with that, but radical self acceptance might be a tall order for a 4 week childbirth class. Is there anything else you'd like us to know? I’m here to help and support. I know a lot of community resources that I can point folks to. I can work out payment plans if need be. I offer discounts to people on OHP and BIPOC who are at risk of poorer health outcomes related to racial discrimination. How can I sign up for Stephanie's classes? www.elliottlactation.com/classes You can register on the site linked above and pay via credit card or apple pay. You’ll get an email from Stephanie shortly after confirming and a few weeks before class you’ll get a login for the online learning platform. Stephanie's next childbirth education, breastfeeding, and newborn care series begins on Sunday, May 19th, 2019, and goes for four weeks, so, sign up soon! How can I contact Stephanie? Facebook: www.facebook.com/elliottlactation IG: @elliottparenteducation [email protected] 503-515-7246 Kestrel, tell us a little bit about yourself - both personal and professional.
While I have been engaged in the childbearing realm since the first birth I attended in 1997, it was both my own postpartum experiences as well as listening to the triumphs and struggles of other mothers that inspired me to write the Build Your Nest postpartum planning workbook. I wrote it as a mother for other parents. I knew people needed a tool that empowered them to make their own plan, not just more information. I live on the Oregon coast and am active in my community supporting breastfeeding as a La Leche League leader. How did you become passionate about the postpartum period? After my son was born, almost 12 years ago, I made the completely erroneous assumption that because birth is natural, that recovery and early mothering should just happen naturally, without any special considerations or time off from our family business and creative life. My recovery was anything but easy. So when I was pregnant for the second time 8 years ago, I began researching and found that there are postpartum traditions from all continents that celebrate and care for mothers after birth. I called my mother-in-law who affirmed this with her own experience birthing in Vietnam during the war. I was struck by the idea that women in Vietnam giving birth in the context of war and poverty received better care than most American women. So, I made a simple postpartum plan and had a completely different experience of recovery and bonding with my daughter. This inspired me to share this with others. How can this book help clients prepare for the postpartum period? The workbook gives important information about the postpartum time and walks them through all aspects of their lives -which of course a newborn changes everything! It asks questions. It offers lots of ideas. It encourages people to engage with the planning process in their own way and make a plan that is truly right for them. What is a postpartum plan? A postpartum plan lays out how you are going to get the rest, support and care you need after giving birth. This includes the Milk Retreat - a set amount of time for having rest, support, and care. And a “Postpartum Net” which is the contingency part of the plan - what resources do you have for the challenges that may arise. We can plan for what we want and be prepared for the unexpected. Where can I find the Build Your Nest postpartum planning workbook? The workbook can be purchased online here: https://www.amazon.com/Build-Your-Nest-postpartum-planning/dp/153361038X/ref=sr_1_1?ie=UTF8&qid=1549153717&sr=8-1&keywords=build+your+nest+workbook. It can also be purchased in Portland, Oregon, at both Milagros and Zenana Spa. We also have them for sale in our Unfurling Birth office. For more info about Kestrel Gates and the Build Your Nest postpartum planning workbook, look here: www.BuildYourNestWorkbook.com Have you used the Build Your Nest Postpartum Planning Workbook? If so, leave us a comment about what you like about it or how it helped you plan! We're excited to be offering a series of interviews on our blog over the coming months. Starting us off, later this month we'll hear from a dear friend and postpartum planning specialist, Kestrel Gates, with her Build Your Nest Postpartum Planning Workbooks. You will not want to miss this interview!
Are you a complementary care provider (a prenatal/postpartum mental health specialist, a lactation consultant, an acupuncturist specializing in fertility or induction, a birth photographer, etc?) Would you like to be interviewed on our blog? Please reach out to us at [email protected] for an interview! Are you a client of ours who would like to be interviewed about their pregnancy, labor, birth, and/or postpartum experience? Reach out to us and let us know! We'd love to interview you! We hope to hear from some of you soon! Stay tuned for the first post coming up soon, and comment here if there's someone you'd like to hear an interview from! xo, Catherine and Maura |
AuthorCheck out Catherine's bio using the button below! Archives
December 2023
Categories |
Photography by Meg Ross Photography, Tanya Hladik, @mindfulwayfarer, @dijanaszewczyk, and Chelsea Jones



































 RSS Feed
RSS Feed